This article was written by Isaac Olushola, Youth RISE’s Global Fund Project Manager.
The Silent Killer – Hepatitis B
In the vast landscape of global health, there are diseases that quietly wreak havoc, often overlooked until they strike with devastating consequences. One such silent killer is Hepatitis B, a preventable disease caused by the hepatitis B virus (HBV). This insidious virus, despite the availability of a vaccine, continuously claims lives, with over 820,000 preventable deaths reported annually.
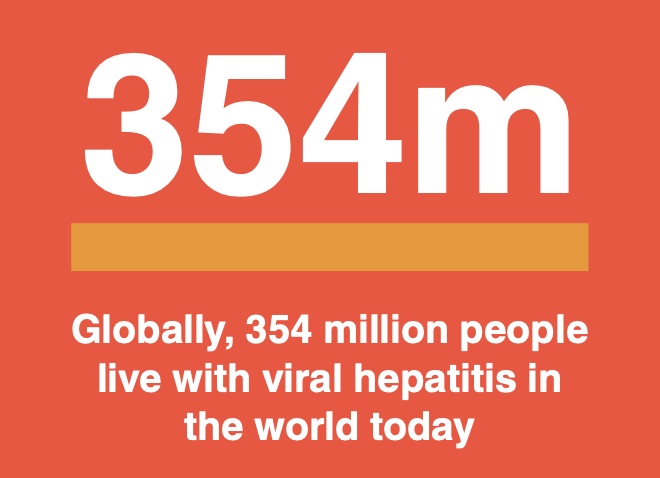
The World Health Organisation (WHO) estimates that nearly 300 million people worldwide live with this virus. The majority of these infections occur in infancy and early childhood, leading to chronic hepatitis in about 95% of cases. Chronic HBV infection is not benign; it significantly increases the risk of progressive liver damage, disease and cancer and may ultimately lead to death. The gravity of this situation is further underscored when we consider that the virus is most commonly spread from mother to child during birth and through contact with the bodily fluids of an infected Individual. This means that the most vulnerable among us – infants and children – are at the highest risk of developing chronic HBV infection.
The WHO has set an ambitious goal to end viral hepatitis as a public health problem by 2030. Achieving this target requires up-to-date national and sub-national data on infection levels. However, most low- and middle-income countries, including Nigeria, lack reliable data due to inadequate disease surveillance, ill-equipped laboratories, and poor healthcare services.
Indeed, the reliable data gap is a barrier in the fight against hepatitis B. Without accurate information on the number of people infected with HBV, it becomes exceedingly difficult to design effective public health control measures. This is a critical issue that needs to be addressed if we are to make any significant progress in combating this silent killer.
In Nigeria, this situation is particularly alarming as recent data reveals that approximately 9.5% of the population, nearly 20 million Nigerians, are living with HBV. This high prevalence rate, which varies across different geographical areas, underscores the potential liver disease crisis in the country and the urgent need for targeted prevention and care efforts.
Moreover, the lack of a cure for hepatitis B further complicates matters. While medications are available to reduce the viral load and slow the progression of liver cancer, these treatments are not a cure. Once a person is infected with HBV, they live with the virus for the rest of their lives, constantly managing their symptoms and living with the fear of potential liver damage.
The fight against hepatitis B is a complex challenge that requires a multi-faceted approach. It is not enough to simply focus on treatment; we must also prioritize prevention and early detection. Only then can we hope to make significant strides in our battle against this silent killer.
The Roadblocks to Hepatitis B Elimination
In Nigeria, the fight against hepatitis B is a complex and multifaceted battle, fraught with challenges that extend beyond the medical realm. These challenges, deeply rooted in cultural beliefs, societal attitudes, and systemic disparities in healthcare, pose significant roadblocks to eliminating the infection.
One of the most significant challenges is the cultural beliefs that create barriers to HBV care. In many communities, deeply ingrained cultural and religious beliefs can lead to misconceptions about the disease, contributing to stigma and discrimination against those infected. For instance, in some rural communities, HBV is often associated with spiritual curses or witchcraft, leading to a reluctance to seek medical treatment. Instead, traditional healers are often consulted, resulting in delayed diagnosis and treatment that aggravates their conditions.
Furthermore, stigma and discrimination are notable barriers that prevent people from accessing health services. Those living with HBV often face social ostracization, which can lead to psychological distress and deter medical help-seeking. This is particularly true for marginalized populations who are vulnerable to HBV, such as people who inject drugs. These individuals often face double discrimination – for their drug use and their HBV status – leading to their exclusion from testing and clinical care.
Access to healthcare services is another significant challenge where the allocation of healthcare resources in Nigeria is skewed towards secondary and tertiary services, which are mostly concentrated in urban areas. This leaves rural areas, where HBV infection rates are higher, underserved and vulnerable. The lack of healthcare facilities in these areas shows that many individuals may have to travel long distances to access testing and treatment services, which can be both time-consuming and cost-ineffective. Despite the existence of a national response to viral hepatitis, less than 5% of people with viral hepatitis B have ever used clinical services. This low uptake of clinical services is a testament to the multitude of barriers that prevent individuals from accessing the care they need.
People who inject drugs face double discrimination – for their drug use and their HBV status – leading to exclusion from testing and clinical care.
Additionally, the situation is even more dire for refugees and people living in hard-to-reach communities. These individuals often live in conditions that make them particularly susceptible to HBV infection, such as overcrowded living conditions and lack of access to clean water and sanitation facilities. Concurrently, they face significant barriers to accessing healthcare services, including geographical isolation, lack of transportation, and financial constraints.
Addressing these challenges requires a comprehensive approach that not only focuses on improving healthcare services but also addresses the social and cultural factors that contribute to the spread of HBV. It requires concerted efforts from all stakeholders – from policymakers and healthcare providers to community leaders and individuals – to create an environment where everyone, regardless of their socio-economic status or geographical location, can access the care they need.
Accelerating the Fight Against Hepatitis B
The 2023 World Hepatitis Day themed, “We’re not waiting,” is a call to action to accelerate concerted and elimination efforts of viral hepatitis. It emphasizes the urgent need for upscaling testing and treatment services for those who need it most. For Nigeria, this means improving identification and testing, and integrating treatment as part of routine care, along with vaccination to prevent new infections. It also involves improving access to prevention and care for rural populations, who make up a significant community of people with HBV in Nigeria.
To avert a liver disease crisis in Nigeria, it is critical to conduct early diagnosis of all Nigerians infected with hepatitis B and provide them with appropriate care. This requires adequate funding through national health budgets to minimize out-of-pocket costs and ensure access to relevant services without incurring financial hardship on individuals as a tenet of achieving Universal Health coverage.
In February 2020, the Nigerian government, along with other African Union member states, pledged to eliminate hepatitis as a public health threat by 2030. Despite the challenges posed by COVID-19, Nigeria can ward off hundreds of thousands of preventable deaths with renewed political commitments, clearly defined targets, and financial support.
As we commemorate World Hepatitis Day, we call on everyone to take action because Hepatitis Can’t Wait. We must unite to make our voices heard, celebrate the progress we have made and meet the current challenges. Let’s increase awareness and encourage real political change to facilitate prevention, diagnosis, and treatment. Collectively, we can make hepatitis elimination a reality.